Pancreatic and Biliary Cancer
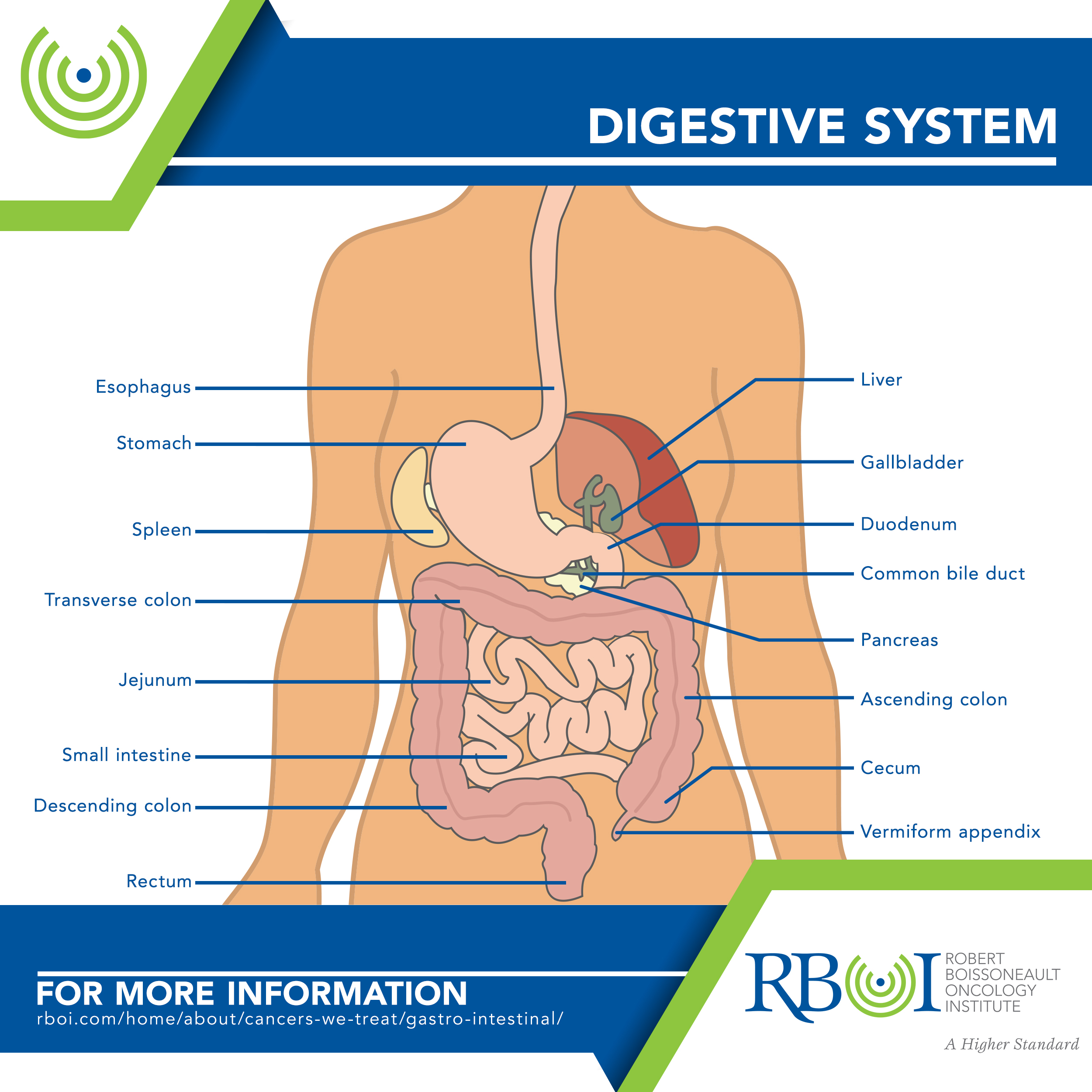
The pancreas is an organ that sits behind the stomach. Pancreatic cancer can start in one of two types of cells in the pancreas: (1) exocrine cells, which make enzymes that help the body digest food; and (2) endocrine (also called neuroendocrine) cells, which make hormones, most importantly insulin.
The biliary system refers to the liver, gall bladder, and bile ducts.
- The liver lies under the right ribs just beneath the right lung. This page describes cancer that develops in the liver (called primary liver cancer), as opposed to cancer that has spread (metastasized) to the liver from elsewhere.
- The gallbladder is located under the liver and stores bile, a fluid made in the liver. Gallbladder cancer is rare.
- The bile ducts are thin tubes that transport bile from the liver and gallbladder into the small intestine, for help in digesting fats in food. Bile duct cancer is also called cholangiosarcoma.
-
Forms of pancreatic and biliary system cancer
Exocrine tumors are the most common type of pancreatic cancer.
Adenocarcinomas account for about 95 percent of exocrine pancreatic cancers and usually start in the ducts of the pancreas.
Intraductal papillary mucinous neoplasm (IPMN) is an increasingly common diagnosis. These tumors grow within the ducts of the pancreas and make a thick fluid called mucin. IPMN is not cancerous when it begins but it could become cancerous if not treated.
Much rarer types of exocrine pancreatic tumors include acinar cell carcinoma, adenosquamous carcinoma, colloid carcinoma, giant cell tumor, hepatoid carcinoma, mucinous cystic neoplasms, pancreatoblastoma, serous cystadenoma, signet ring cell carcinoma, solid and pseudopapillary tumors, squamous cell carcinoma, and undifferentiated carcinoma.
Endocrine tumors (also called pancreatic neuroendocrine tumors (PNETs) or islet cell tumors) make up about 7 percent of pancreatic cancers.
Ampullary cancer (carcinoma of the ampulla of Vater) starts where the bile duct and pancreatic duct come together and empty into the small intestine. They often block the bile duct and lead to yellowing of the skin and eyes (jaundice).
Hepatocellular carcinom (HCC) accounts for about 80 percent of primary liver cancers in adults. HCC can have different growth patterns; the most common pattern in the US is tentacle-like growths throughout the liver. Other patterns include a single tumor that grows larger, or multiple nodules in several different places in the liver. A rare subtype of HCC, fibrolamellar, is usually seen in women younger than age 35.
Angiosarcomas account for about 1 percent of primary liver cancers in adults. They start in the blood vessels of the liver and grow very quickly.
Hepatoblastoma is a very rare liver cancer that develops in children who are usually younger than 4 years old.
Gallbladder cancers are rare and nearly all of them are adenocarcinomas.
- Papillary adenocarcinoma (also called papillary cancer) is a rare type of gallbladder adenocarcinoma. Papillary cancers are usually less likely to spread into the liver or nearby lymph nodes and tend to have a better prognosis than most other kinds of gallbladder adenocarcinomas.
- Other cancers that can start in the gallbladder include adenosquamous carcinomas, squamous cell carcinomas, and carcinosarcomas but these are very rare.
Bile duct cancers include intrahepatic (starting inside the liver) and extrahepatic (starting outside the liver).
- Intrahepatic cholangiocarcinoma accounts for about 10 to 20 percent of cancers that start in the liver. However, most cholangiocarcinomas start in the bile ducts outside the liver.
- Perihilar (or hilar) bile duct cancers, also called Klatskin tumors, start where the left and right hepatic ducts have joined and are just leaving the liver.
- Distal bile duct cancers occur further down the bile duct, closer to the small intestine.
-
Risk factors for pancreatic cancer
Age, Alcohol, Bacteria, Chemical exposure and environmental factors, Chronic pancreatitis, Cirrhosis, Diabetes, Family history, Gender, Obesity/diet, Race/ethnicity, Rare inherited conditions, Smoking, Viral hepatitis
Age — Risk increases with age, though adults can be diagnosed at any age. Among those diagnosed, 90 percent are older than 55 and 70 percent are older than 65.
Alcohol — Chronic, heavy alcohol use can lead to conditions like chronic pancreatitis, which increases risk.
Bacteria — Infection with Helicobacter pylori (H. pylori) may increase risk. More research is needed.
Chemical exposure and environmental factors — Exposure to certain chemicals such as pesticides, benzene, certain dyes, and petrochemicals may increase the risk of developing pancreatic cancer.
Chronic pancreatitis — Some research suggests that having chronic pancreatitis may increase the risk of developing pancreatic cancer.
Cirrhosis — Most cirrhosis in the US is caused by alcohol abuse (see Alcohol, above). Other causes include nonalcoholic fatty liver disease (NAFLD), viral hepatitis, hemochromatosis, and other rare types of chronic liver disease.
Diabetes — Many studies have indicated that diabetes, especially when a person has had it for many years, increases risk. Most of the risk is found in people with type 2 diabetes. Suddenly developing diabetes later in adulthood can be an early symptom of pancreatic cancer.
Family history — You and your family may be at risk if 2 or more first-degree relatives (parents, children, siblings) or at least 3 members of the family have been diagnosed with pancreatic cancer.
Gender — More men than women are diagnosed.
Obesity/diet — Obese and even overweight people are at higher risk. Obese people are about 20% more likely to develop pancreatic cancer. Regularly eating high-fat foods is a risk factor.
Race/ethnicity — Pancreatic cancer risk is higher in African Americans (compared with Asian, Hispanic, or white people) and in people of Ashkenazi Jewish descent.
Rare inherited conditions — Risk increases significantly for members of families with hereditary pancreatitis (HP), Peutz-Jeghers syndrome (PJS), Familial malignant melanoma and pancreatic cancer (FAMM-PC), Hereditary breast and ovarian cancer (HBOC) syndrome, Lynch syndrome, Li-Fraumeni syndrome (LFS), and/or Familial adenomatous polyposis (FAP).
Smoking — People who smoke are 2 to 3 times more likely to develop pancreatic cancer than those who don’t. About 25 percent of pancreatic cancers are thought to be caused by cigarette smoking.
Viral hepatitis — One study has shown that a previous hepatitis B infection was twice as common in people with pancreatic cancer than in those without the cancer. More research is needed.
-
Risk factors for liver cancer
Age, Alcohol, Anabolic steroids, Chemical exposure and environmental factors, Cirrhosis, Diabetes, Gender, Obesity/diet, Race/ethnicity, Rare diseases, Smoking, Viral hepatitis
Age — In the US, primary liver cancer occurs most often in people older than 60.
Alcohol — Alcohol abuse is a leading cause of cirrhosis in the US, which in turn is linked with an increased risk of liver cancer.
Anabolic steroids — Long-term anabolic steroid use can slightly increase the risk of hepatocellular cancer (HCC). Cortisone-like steroids, such as hydrocortisone, prednisone, and dexamethasone, do not carry this same risk.
Chemical exposure and environmental factors — Exposure to certain chemicals (such as vinyl chloride and thorium dioxide (Thorotrast)), or eating food contaminated with aflatoxin (a mold that can grow on stored nuts and grains), may increase risk. There is less risk of aflatoxin in the US. Thorotrast is no longer used, and exposure of workers to vinyl chloride is strictly regulated.
Cirrhosis — Combined alcohol abuse and hepatitis virus infection puts people at high risk of both cirrhosis and hepatocellular carcinoma (HCC).
Diabetes — Strong evidence suggests that diabetes is a risk factor for hepatocellular carcinoma (HCC) in the US.
Gender — Hepatocellular carcinoma (HCC) is much more common in men than in women.
Obesity/diet — Obesity can lead to nonalcoholic fatty liver disease (NAFLD), which strong evidence suggests is a risk factor for hepatocellular carcinoma (HCC) in the US.
Race/ethnicity — In the US, Asian Americans and Pacific Islanders have the highest rates of liver cancer, followed by Hispanics/Latinos, American Indians/Alaska Natives, African Americans, and whites.
Rare diseases — Diseases that increase the risk of liver cancer include: Tyrosinemia, Alpha1-antitrypsin deficiency, Porphyria cutanea tarda, Glycogen storage diseases, Wilson disease.
Smoking — Smoking increases the risk of liver cancer. Former smokers have a lower risk than current smokers, but both groups have a higher risk than those who never smoked.
Viral hepatitis — Viral hepatitis is the largest risk factor for liver cancer worldwide. Hepatitis C has become much more common than hepatitis B because there is no vaccine to prevent hepatitis C. If you develop acute hepatitis B or C and then “clear the virus,” you have no increased risk of liver cancer. Only people who do not clear the virus and have a persistent infection have an increased risk.
-
Risk factors for gallbladder cancer
Age, Bacteria, Bile duct abnormalities, Choledochal cysts, Family history, Gallbladder polyps, Gallstones/bile duct stones, Gender, Obesity/diet, Porcelain gallbladder, Primary sclerosing cholangitis (PSC), Race/ethnicity, Smoking
Age — Most people diagnosed with gallbladder cancer are older than 70.
Bacteria — People chronically infected with salmonella (the bacterium that causes typhoid) and those who are carriers of typhoid are more likely to get gallbladder cancer than those not infected.
Bile duct abnormalities — People with abnormalities that cause fluids from the pancreas to flow backward (reflux) into the bile ducts are at higher risk of gallbladder cancer.
Choledochal cysts — The cells lining these bile-filled sacs often have areas of pre-cancerous changes, which can progress to gallbladder cancer over time.
Family history — A family history of gallbladder cancer slightly increases the risk of developing gallbladder cancer.
Gallbladder polyps — Doctors often recommend gallbladder removal for people who have polyps larger than 1 centimeter because these are more likely to be cancerous.
Gallstones/bile duct stones — Gallstones are the most common risk; 75 to 90 percent of people with gallbladder cancer have a history of gallstones. However, less than 1 percent of people with gallstones develop gallbladder cancer.
Gender — In the US, gallbladder cancer occurs 3 to 4 times more often in women than in men.
Obesity/diet — Patients with gallbladder cancer are more often overweight or obese than people without this disease. Obesity is also a risk factor for gallstones, which might help explain this link.
Porcelain gallbladder — People with this condition have a higher risk of developing gallbladder cancer.
Primary sclerosing cholangitis (PSC) — People with PSC (inflamed bile ducts) have an increased risk of gallbladder and bile duct cancer.
Race/ethnicity — Mexican Americans and Native Americans, particularly in the southwestern United States, are more likely to develop gallbladder cancer than the general population.
Smoking — Tobacco use may increase risk.
-
Risk factors for bile duct cancer
Age, Alcohol, Bile duct abnormalities, Caroli syndrome, Chemical exposure and environmental factors, Choledochal cyst, Chronic pancreatitis, Cirrhosis, Diabetes, Family history, Gallstones/bile duct stones, Inflammatory bowel disease (IBD), Liver flukes, Obesity/diet, Primary sclerosing cholangitis (PSC), Race/ethnicity, Smoking, Viral hepatitis
Age — Most people diagnosed with bile duct cancer are in their 60s or 70s.
Alcohol — People who drink alcohol are more likely to get intrahepatic bile duct cancer. The risk is higher in those who have liver problems from drinking alcohol.
Bile duct abnormalities — People with abnormalities that cause fluids from the pancreas to flow backward (reflux) into the bile ducts are at higher risk of bile duct cancer.
Caroli syndrome — This abnormality increases the risk of infection and stones, like gallstones.
Chemical exposure and environmental factors — Dioxins, nitrosamines, and polychlorinated biphenyls (PCBs), as well as exposure to thorium dioxide (Thorotrast, no longer used), may cause bile duct cancer. In particular, people who work in rubber plants and automotive industries may be exposed more often to these chemicals.
Choledochal cyst — The cells lining these bile-filled sacs often have areas of pre-cancerous changes, which can progress to bile duct cancer over time.
Chronic pancreatitis — Chronic pancreatitis might increase risk, but more research is needed.
Cirrhosis — Studies have found that cirrhosis increases the risk of bile duct cancer.
Diabetes — People with diabetes (type 1 or type 2) have a higher risk of bile duct cancer. This increase in risk is not high, and the overall risk of bile duct cancer in someone with diabetes is still low.
Family history — A family history of bile duct cancer seems to increase risk. However, risk is low because this is a rare disease. Most bile duct cancers are not found in people with a family history of the disease.
Gallstones/bile duct stones — Bile duct stones, which are a lot like but much smaller than gallstones, can also cause inflammation that increases the risk of bile duct cancer.
Inflammatory bowel disease (IBD) — People with diseases like ulcerative colitis and Crohn’s disease have an increased risk of bile duct cancer.
Liver flukes — These parasites can infect the bile duct. Liver flukes most closely related to bile duct cancer risk are Clonorchis sinensis and Opisthorchis viverrini.
Obesity/diet — Being overweight or obese can increase the risk of bile duct cancer. This could be because obesity increases the risk of cancer precursors, such as bile duct stones, non-alcoholic fatty liver disease (NAFLD), and hormonal changes.
Primary sclerosing cholangitis (PSC) — Bile duct stones, which are a lot like but much smaller than gallstones, can also cause inflammation that increases the risk of bile duct cancer.
Race/ethnicity — In the US, the risk of bile duct cancer is highest among Hispanic Americans.
Smoking — Smoking might increase risk, but more research is needed.
Viral hepatitis — Infection with hepatitis B virus or hepatitis C virus increases the risk of intrahepatic bile duct cancers. This may be at least in part because long-term infections with these viruses can also lead to cirrhosis.
-
Symptoms of pancreatic and biliary system cancer
Pancreatic cancer is called a “silent disease” because there are few noticeable symptoms early on. There are currently no specific tests that can reliably find pancreatic cancer for people who do not have symptoms.
As the cancer grows, symptoms may include:
- Jaundice (yellow skin and eyes), darkening of the urine, itching, and clay-colored stool.
- Pain in the upper abdomen or upper back
- Painful swelling of an arm or leg due to a blood clot
- Burning feeling in stomach or other gastrointestinal discomforts
- Stomach bloating
- Gallbladder or liver enlargement
- Floating stools with a particularly bad odor and an unusual color, due to the body not digesting fats well
- Weakness
- Loss of appetite
- Unexplained weight loss
- Nausea and vomiting
- Chills
- Fever
- Diabetes
Note that symptoms may be caused by a medical condition other than cancer.
People with liver cancer (mainly hepatocellular carcinoma, or HCC) may experience no symptoms, particularly when the tumor is detected early as part of a screening program. When symptoms or signs do occur, they include:
- Pain, especially at the top right of the abdominal area, near the right shoulder blade, or in the back
- Unexplained weight loss
- A hard lump under the ribs on the right side of the body, which could be the tumor or a sign that the liver has gotten bigger
- Swelling or fluid build-up in the abdomen (belly)
- Weakness or fatigue
- Loss of appetite
- Feeling very full after a small meal
- Nausea or vomiting
- An enlarged spleen, felt as fullness under the ribs on the left side
- Jaundice (yellowing of the skin and eyes), itching.
Other symptoms can include fever, enlarged veins on the belly that can be seen through the skin, and abnormal bruising or bleeding.
People who have chronic hepatitis or cirrhosis might feel worse than usual or might just have changes in lab test results.
Some liver tumors make hormones that act on organs other than the liver and can cause:
- High blood calcium levels (hypercalcemia), which can cause nausea, confusion, constipation, weakness, or muscle problems
- Low blood sugar levels (hypoglycemia), which can cause fatigue or fainting
- Breast enlargement (gynecomastia) and/or shrinkage of the testicles in men
- High counts of red blood cells (erythrocytosis), which can cause someone to look red and flushed
- High cholesterol levels
Note that symptoms may be caused by a medical condition other than cancer.
Gallbladder cancer doesn’t usually cause signs or symptoms until later in the course of the disease, when the tumor is large and/or has spread. But sometimes symptoms can appear sooner and lead to an early diagnosis.
Some of the more common symptoms of gallbladder cancer include:
- Abdominal (belly) pain and cramping, usually in the upper right part of the belly
- Lumps on the right side of the belly
- Nausea and/or vomiting
- Jaundice
Less common symptoms of gallbladder cancer include:
- Loss of appetite
- Unexplained weight loss
- Swelling in the abdomen (belly)
- Fever
- Itchy skin
- Dark urine
- Light-colored or greasy stools
Gallbladder cancer is rare. These symptoms are more likely to be caused by something other than gallbladder cancer.
Bile duct cancer does not usually cause signs or symptoms until later in the course of the disease, but sometimes symptoms can appear sooner and lead to an early diagnosis. When bile duct cancer does cause symptoms, it’s usually because a bile duct is blocked.
Symptoms may include:
- Jaundice (yellowing of the skin and the whites of the eyes); this is the most common symptom
- Itching
- Unexplained weight loss
- Loss of appetite
- Abdominal pain, especially below the ribs on the right side
- Light colored/greasy stools
- Dark urine
- Fever, nausea, and vomiting, which may occur in people who develop an infection as a result of bile duct blockage. Bile duct cancer is rare. These symptoms are far more likely to be caused by something other than bile duct cancer.
-
How is pancreatic and biliary system cancer treated with radiation?
Pancreatic Cancer
External-beam radiation therapy (EBRT) is the type of radiation therapy used most often for pancreatic cancer.
- Radiation may be used before surgery (and with chemotherapy) to try to shrink the cancer and make it easier to remove.
- Radiation may be used after surgery (and with chemotherapy) to try to kill any areas of cancer cells that may have been left behind but are too small to see.
- Radiation therapy combined with chemotherapy may be used as part of the main treatment in people whose cancers have grown beyond the pancreas and can’t be removed by surgery.
- Radiation may be used as palliative therapy to help relieve symptoms (such as pain) in people with advanced cancers or in people who aren’t healthy enough for other treatments like surgery.
Pancreatic cancer can be treated with (1) traditional radiation therapy; (2) stereotactic body radiation therapy (SBRT), also called Cyberknife, which delivers high doses of radiation to a tumor while limiting the amount of radiation going to healthy tissues; or (3) proton beam therapy, which uses protons rather than X-rays.
Liver Cancer
External-beam radiation therapy (EBRT) is the type of radiation therapy most often used to treat adult primary liver cancer. Radiation may be used for:
- Liver cancer that cannot be removed by surgery.
- Liver cancer that cannot be treated
- Liver cancer that has spread to other areas such as the brain or bones.
- Treating pain caused by large liver cancers.
- People with a tumor thrombus (a collection of liver cancer cells) blocking the portal vein.
Radiation can be delivered externally using stereotactic body radiation therapy (SBRT). SBRT includes several methods of delivering high doses of radiation to a tumor while limiting the amount of radiation going to healthy tissues. Another technique, proton beam therapy, uses protons rather than X-rays.
Radiation may also be delivered internally via a technique called radioembolization. Small radioactive beads are injected into the hepatic artery. The beads then lodge in the liver near the tumor and give off small amounts of radiation that travel only a short distance.
Radiation may not be a good option for some patients whose liver has been greatly damaged by diseases such as hepatitis or cirrhosis.
Gallbladder Cancer
External-beam radiation therapy (EBRT) is the type of radiation therapy most often used to treat gallbladder cancer. In gallbladder cancer patients, radiation is usually combined with chemotherapy. Often, special types of external beam radiation, such three-dimensional conformal radiation therapy (3D-CRT) and intensity modulated radiation therapy (IMRT) are used, to limit damage to nearby normal tissues.
- Radiation may be used after surgery to try to kill any areas of cancer cells that may have been left behind but are too small to see.
- Radiation may be used as a main therapy for some patients whose cancer has not spread widely throughout the body, but can’t be removed with surgery. While treatment in this case does not cure the cancer, it may help patients live longer.
- Radiation may be used as palliative therapy to help relieve symptoms (such as pain) in people with advanced cancers, by shrinking tumors that block blood vessels or bile ducts or that press on nerves.
Bile Duct Cancer
External-beam radiation therapy (EBRT) is the most common form of radiation for bile duct cancer. However, internal radiation therapy (brachytherapy) may also be used.
- Radiation may be used before surgery to try to shrink the cancer and make it easier to remove.
- Radiation may be used after surgery to try to kill any areas of cancer cells that may have been left behind but are too small to see.
- Radiation may be used as a main therapy for some patients whose cancer has not spread widely throughout the body, but can’t be removed with surgery. While treatment in this case does not cure the cancer, it may help patients live longer.
- Radiation may be used as palliative therapy — to help relieve symptoms (such as pain) in people with advanced cancers, by shrinking tumors that block blood vessels or bile ducts or that press on nerves.
It is not clear how helpful radiation is when used either before or after surgery for bile duct cancer.
Often, special types of external beam radiation, such as three-dimensional conformal radiation therapy (3D-CRT), intensity modulated radiation therapy (IMRT), stereotactic body radiotherapy (SBRT), or chemoradiation are used, to limit damage to nearby normal tissues.
Internal radiation therapy for bile duct cancer uses a technique called intrabiliary brachytherapy, in which a thin radioactive wire is put into the bile duct for a short time. The radiation travels a very short distance, so it affects the cancer without causing much harm to nearby healthy body tissues. Brachytherapy can be used alone, or it may be used along with EBRT. At this time it’s mostly used as a palliative treatment.
Click here to learn more about RBOI’s radiation treatment options
Click here to watch a walk-through of what is involved in radiation treatment at RBOI
More extensive information about pancreatic, biliary system, and other cancers may be found at these sites:
American Cancer Society: Cancer.org
American Society of Clinical Oncology: Cancer.net
National Cancer Institute: Cancer.gov
