Cervical Cancer
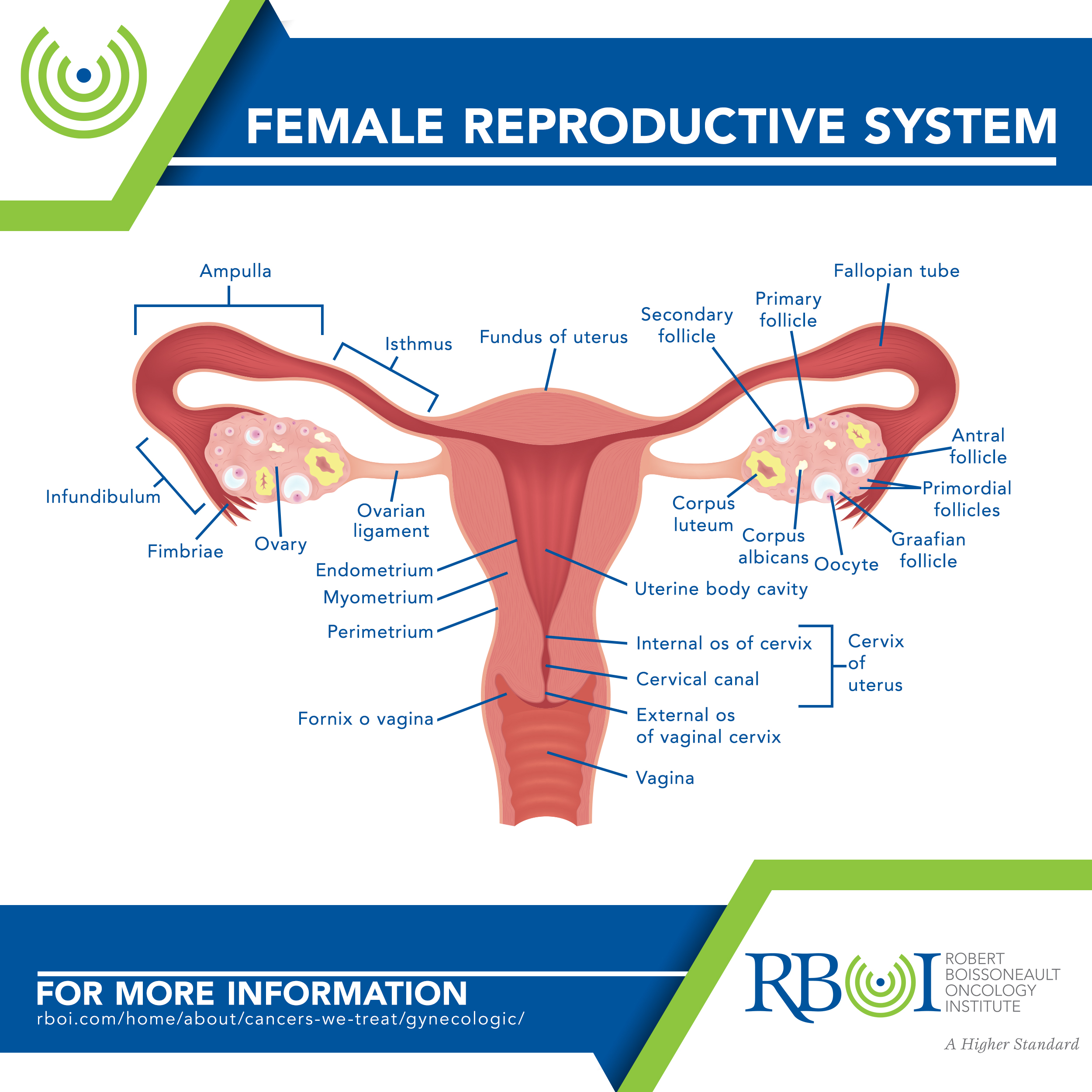
Cervical cancer usually develops slowly over time. It starts in a woman’s cervix, which is the lower, narrow part of the uterus and connects the uterus with the vagina. Before cancer forms, abnormal cells begin to appear in the cervical tissue, a process called dysplasia. Over time, the abnormal cells may become cancer cells and start to grow and spread more deeply into the cervix and to surrounding areas.
-
Forms of cervical cancer
Squamous cell carcinomas account for up to 90 percent of cervical cancers. They usually develop where the exocervix (the part closest to the vagina) joins the endocervix (the part closest to the uterus), a place called the transformation zone.
Adenocarcinomas form most of the other cervical cancers and develop from the mucus-producing gland cells of the endocervix.
Adenosquamous carcinomas (also called mixed carcinomas) are less common and have features of both squamous cell carcinomas and adenocarcinomas.
Rare cervical cancers include melanoma, sarcoma, and lymphoma, which occur more commonly in other parts of the body.
-
Risk factors for cervical cancer
Age, Carrying a full-term pregnancy before age 17, Chlamydia infection, Diet low in fruits and vegetables, Diethylstilbestrol (DES) exposure, Family history of cervical cancer, Having 3 or more full-time pregnancies, Herpes, Human papillomavirus (HPV) infection, Immune system deficiency, Long-term use of oral contraceptives, Smoking, Socioeconomic factors, Weight
Age — The risk of cervical cancer increases between the late teens and mid-30s. Women older than 40 remain at risk and need to continue having regular cervical cancer screenings, including both a Pap test and HPV test.
Carrying a full-term pregnancy before age 17 — Women who gave birth before age 17 are almost twice as likely to get cervical cancer later in life than women who waited to get pregnant until they were 25 years or older.
Chlamydia infection — Some studies have seen a higher risk of cervical cancer in women whose blood tests and cervical mucus showed evidence of past or current chlamydia infection.
Diet low in fruits and vegetables — Fruits and vegetables contain antioxidants, carotenoids, flavonoids, and folate, which can help the body fight off HPV and can prevent an HPV infection from turning cervical cells into cancerous lesions. Women with diets low in fruits and vegetables may be at increased risk for cervical cancer.
Diethylstilbestrol (DES) exposure — DES was given from about 1940 to 1971 to prevent miscarriages. Women whose mothers were given this drug during pregnancy have an increased risk of developing clear-cell adenocarcinoma, a rare type of cancer of the cervix or vagina. DES daughters may also be at increased risk of developing squamous cell cancers and pre-cancers of the cervix linked to HPV. They should have an annual pelvic examination that includes a cervical Pap test as well as a 4-quadrant Pap test, in which all sides of the vagina are checked for abnormal cells.
Family history of cervical cancer — Women whose mother or sister had cervical cancer have a higher chance of developing the disease.
Having 3 or more full-time pregnancies — Women who have had 3 or more full-term pregnancies have an increased risk of developing cervical cancer.
Herpes — Women who have genital herpes have a higher risk of developing cervical cancer.
Human papillomavirus (HPV) infection — There are over 100 different types of HPV, but HPV16 and HPV18 are the types most frequently associated with cervical cancer. The virus is usually contracted through sexual activity with someone who has HPV, and is the most important risk factor for cervical cancer.
Immune system deficiency — Immune suppression from corticosteroid medications, organ transplantation, treatments for other types of cancer, or human immunodeficiency virus (HIV) increase the risk of developing cervical cancer.
Long-term use of oral contraceptives — Some studies suggest that birth control pills may be associated with an increase in cervical cancer risk. Research suggests that the risk of cervical cancer goes up the longer a woman takes oral contraceptives, but then goes back down after the pills are stopped, returning to normal in about 10 years. Other research suggests that women who had ever used an intrauterine device (IUD) had a lower risk of cervical cancer.
Smoking — Women who smoke are about twice as likely to develop cervical cancer as women who do not smoke.
Socioeconomic factors — Women without access to cervical cancer screening are at higher risk. Populations affected include black, Hispanic, and Native American women.
Weight — Overweight women are more likely to develop adenocarcinoma of the cervix.
-
Symptoms of cervical cancer
Light bleeding or spotting between or following periods
Unusually long or heavy menstrual bleeding
Bleeding after sexual intercourse, douching, or a pelvic examination
Bleeding after menopause
Increased vaginal discharge
Pain during sexual intercourse
Unexplained, persistent pelvic and/or back pain
-
How is cervical cancer treated with radiation?
Intensity modulated radiation therapy (IMRT) is a type of 3-dimensional, external beam radiation therapy (EBRT) that can more directly target a tumor. Radiation beams are broken up into smaller beams and the intensity of each of these smaller beams can be changed. IMRT can deliver higher doses of radiation to the tumor while giving less to the surrounding healthy tissue. When used as the main treatment for cervical cancer, IMRT is usually combined with chemotherapy.
Brachytherapy (internal radiation therapy) differs from external beam radiation therapy because a radiation source is placed directly into or near the tumor. The radiation travels a very short distance, so it affects only the tumor. The type of brachytherapy used most often to treat cervical cancer is known as intracavitary brachytherapy. The radiation source is placed in a device in the vagina (and sometimes in the cervix). This is often used in addition to EBRT as a part of the main treatment for cervical cancer.
Radiation may also be used as palliative therapy to relieve symptoms and improve quality of life.
Click here to learn more about RBOI’s radiation treatment options
Click here to watch a walk-through of what is involved in radiation treatment at RBOI
More extensive information about cervical and other cancers may be found at these sites:
American Cancer Society: Cancer.org
American Society of Clinical Oncology: Cancer.net
National Cancer Institute: Cancer.gov
